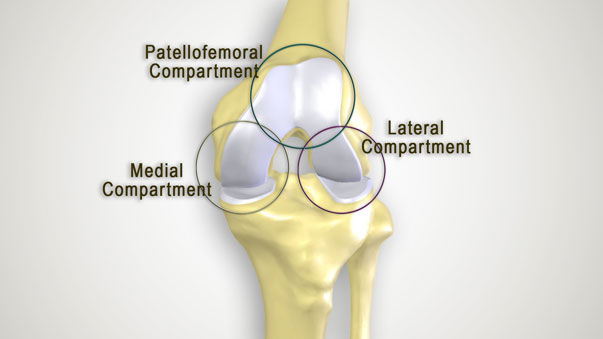
Your knee consists of three “compartments” or sections:
- Medial compartment (inner half of your knee)
- Lateral compartment (outer half of your knee)
- Patellofemoral compartment (behind the knee cap)
Osteoarthritis can affect one, two, or all three compartments. Osteoarthritis (often abbreviated to OA) is a form of arthritis and a degenerative joint disease characterized by the breakdown and eventual loss of joint cartilage. Cartilage is a protein substance that serves as a cushion between the bones of a joint. With OA, the top layer of cartilage breaks down and wears away, allowing bones under the cartilage to rub together.
What causes osteoarthritis of the knee?
Although the root cause of osteoarthritis is unknown, the risk of developing symptomatic Osteoarthritis is influenced by multiple factors such as age, gender and inherited traits that can affect the shape and stability of your joints.
Other factors can include:
- A previous knee injury
- Repetitive strain on the knee
- Improper joint alignment
- Being overweight
- Exercise/sports-generated stress placed on the knee joint
Symptoms of osteoarthritis of the knee include:
- Pain with standing or walking short distances, climbing stairs, getting in and out of chairs
- Pain with activity
- Start-up pain or stiffness when activities are initiated from a sitting position
- Joint stiffness after getting out of bed
- Swelling in one or more areas of the knee
- A grating sensation or crunching feeling in the knee during use
How is osteoarthritis of the knee diagnosed?
Your physician will begin by reviewing your medical history and symptoms. He or she will observe the natural movement of your knee, evaluate your knee and ankle joint alignment, and check your reflexes, muscle strength, range of motion, and ligament stability in the affected knee. Your physician may order X-rays to determine how much joint or bone damage has been done, how much cartilage has been lost, and if there are bone spurs present. Additional medical imaging tests such as computed tomography (CT) or magnetic resonance imaging (MRI) may be ordered to determine exactly where the damage is and its extent. Your physician may also order blood tests to rule out other causes of symptoms or order a joint aspiration which involves drawing fluid from the joint through a needle and examining the fluid under a microscope.
How is osteoarthritis treated?
Whether your osteoarthritis is mild or severe, your physician will most likely recommend certain lifestyle changes to reduce stress on your knee joints such as weight loss. Additional disease and pain management strategies may include physical therapy, steroid injections, over-the-counter pain medications such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), or topical pain-relieving creams. Please speak with your physician if your symptoms aren’t responding to non-surgical solutions, or your pain can no longer be controlled by medication. You could be a candidate for surgery. The most common surgical knee intervention performed for osteoarthritis is a total knee replacement. During this procedure, the diseased bone and cartilage are removed and the joint is resurfaced with an artificial implant. This treatment option is usually offered to patients with advanced osteoarthritis of the knee.
Total knee replacement is not always optimal for patients with early- to mid-stage osteoarthritis in just one or two compartments of the knee. For patients with partial OA of the knee, MAKOplasty® Partial Knee Resurfacing may be the more appropriate solution.
At Hofmann Arthritis Institute, we approach your diagnosis and education with open communication and shared decision-making. It is important that you are fully aware of the effects of osteoarthritis, and know all of the options that are available to you.